Testosterone Replacement Therapy
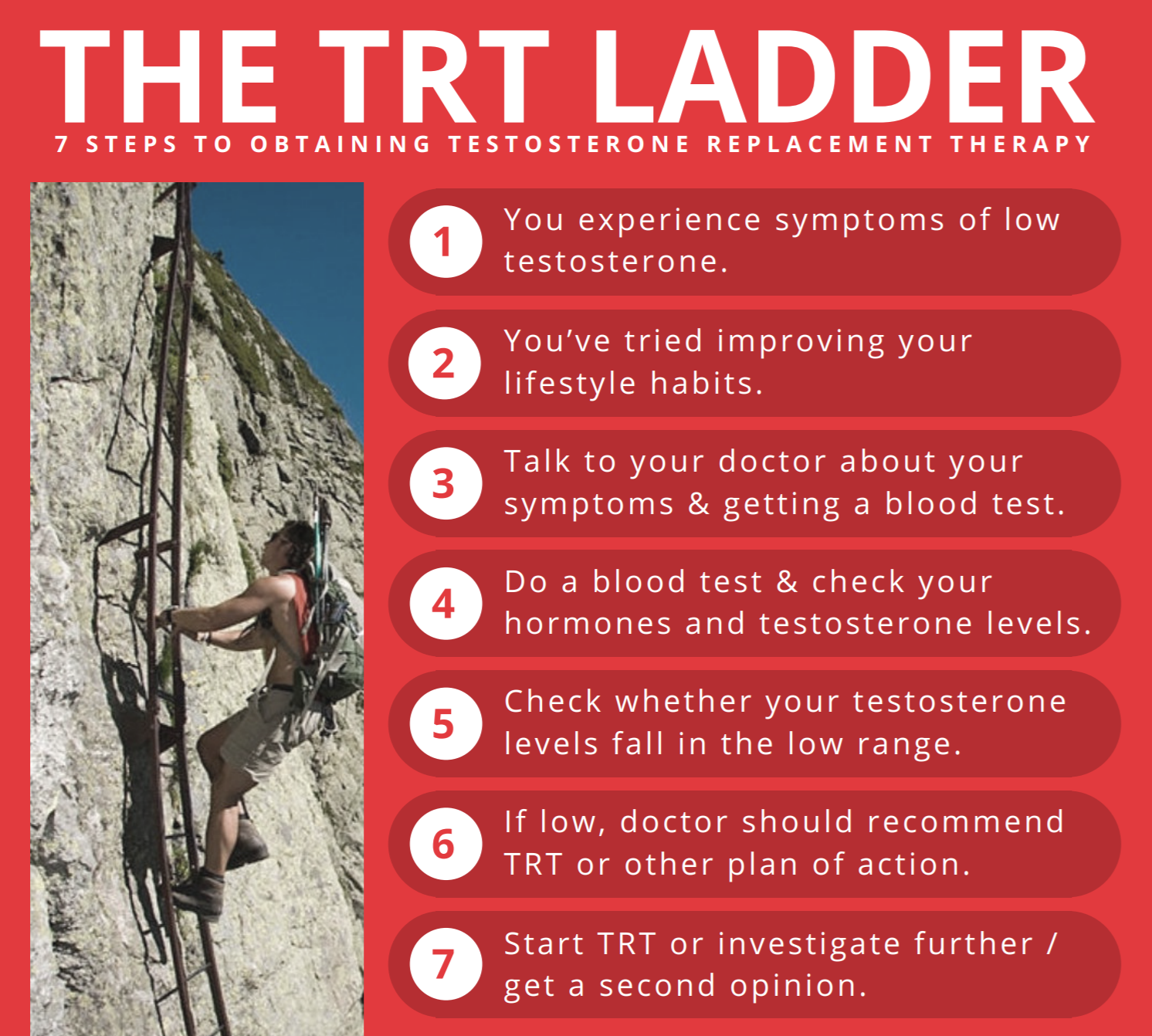
Male Testosterone Replacement Therapy (TRT) is treated by many doctors as taboo. This is mainly due to under-education on the topic, stigma from the public, and fear of litigation in today’s society. Due to liability issues, a large percentage of doctors are not willing to even educate themselves on the matter. In reality, TRT is a valuable treatment modality that can greatly increase quality of life for many men, with minimal risk in otherwise healthy individuals (as long as some precautions are followed). A competent doctor will focus on treating symptoms and root-cause, not numbers on a blood panel.
This compilation intends to provide the most up to date information on all things TRT. Bare in mind that this research does cover supra-physiological use. It is also not intended to diagnose or treat any medical condition, please talk with your physician if you suspect you are a candidate for TRT.

Overview
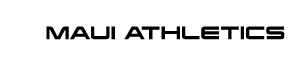
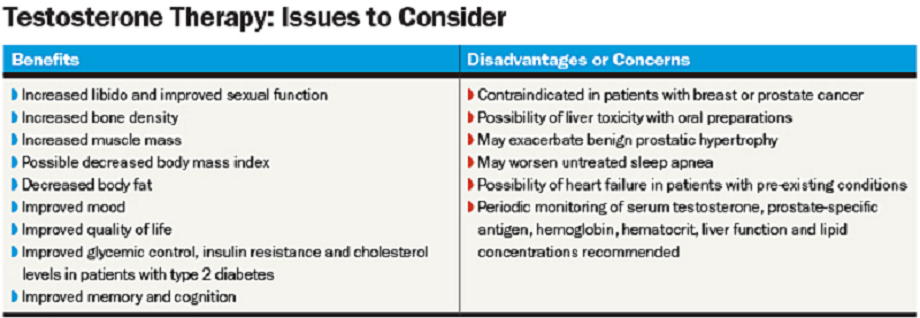
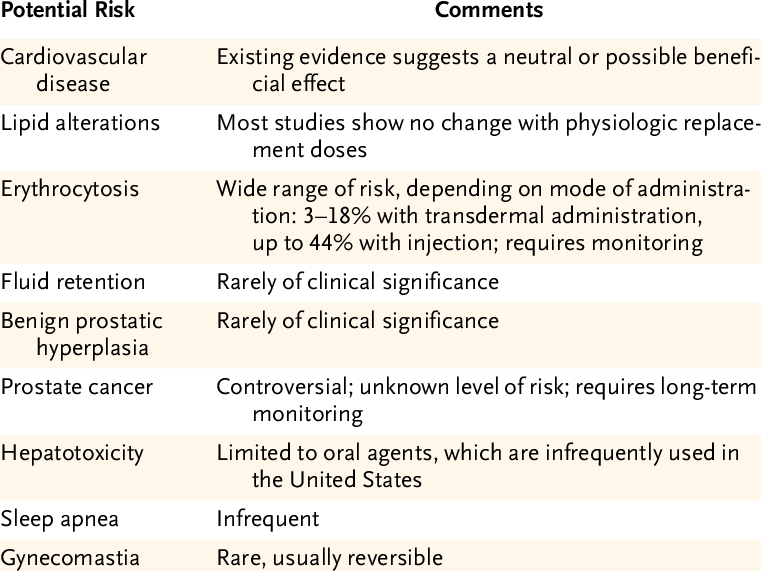
The major benefits of male TRT are increased quality of life, mood, body composition, sexual health, stress management, and much more. The main practical risks come in the forms of infertility, increased estrogen conversion, changes in triglycerides, and erythrocytosis (or an increase in red blood cells). The latter, if not monitored, could lead to a cardiovascular event. There is also the potential for increased severity of certain types of cancer (estrogen replacement therapy for females shares this same concern, but is not nearly as stigmatized).
Testosterone preparations come in various forms (injectable, cream, pellet, etc). My number one recommendation is always injectable as you can more safely and accurately tailor the dose to your own body. Testosterone is generally bound to an ester in injectable form. The type of ester yields vastly different speeds of absorption. Fast acting (short-acting) esters such as Propionate produce higher blood levels much quicker, but also come at the risk of more side-effects.
One such side is the aforementioned erythrocytosis. This is why longer esters such as Cypionate or Enanthate (or in the future Undecanoate) are typically used for TRT. Benefits of these long-acting esters include decreased side effects/risks as well as the requirement for less frequent injections. Another way to mitigate red blood cell production (and estrogen conversion) is to inject smaller doses more frequently to produce smaller blood level spikes of testosterone. Blood panels to monitor hematocrit are of paramount importance during TRT. Luckily, a therapeutic phlebotomy can take care of the issue of erythrocytosis should the need arise. The trick is regular monitoring to catch this before it becomes a significant problem. In many following a TRT dosing protocol, this is never an issue.
When monitoring estrogen conversion, especially in men, I recommend an E sensitive test rather than the standard E test. Standard estrogen tests can give false values as they can be altered by C-reactive protein. E sensitive tests take this into account and provide a more reliable reading.
Diagnosis
Benefits
Risks
All graphics credited to their respective authors.
Research
“Testosterone has a dose-dependent stimulatory effect on erythropoiesis that is more pronounced in older men. The testosterone-induced rise in hemoglobin and hematocrit and age-related differences in response to testosterone therapy may be mediated by factors other than erythropoietin and soluble transferrin receptor levels.” Many studies like this will show that it is imperative to monitor hematocrit levels via routine blood-work while on TRT. This is very important for risk management.
https://www.ncbi.nlm.nih.gov/pubmed/18160461
“Short-acting injectable testosterone is associated with greater risk of erythrocytosis compared with other formulations. The mechanism of the pathophysiology and its role on thrombo-embolic events remain unclear, although some data support an increased risk of cardiovascular events resulting from testosterone-induced erythrocytosis.” This is not surprising given our previous discussion on the action of short vs long acting esters (and a main reason for my recommendation for routine blood work).
https://www.ncbi.nlm.nih.gov/pubmed/28526632
A cohort study by Walsh et al. (2018) followed male Veterans aged 40 to 89 years with a laboratory-defined low testosterone measurement from 2002 to 2011 and recent prostate specific antigen (PSA) testing; excluding those with recent testosterone treatment, prostate or breast cancer, high PSA or prior prostate biopsy. Of the 147,593 men included, 58,617 were treated with testosterone replacement therapy. “Among men with low testosterone levels and normal PSA, testosterone treatment was not associated with an increased risk of aggressive or any increased risk of prostate cancer.” Walsh continued: “This finding doesn’t change the guidelines for how we recommend testosterone therapy. Men should still have their testosterone diagnosed appropriately, with multiple readings, and be counseled about risks and benefits of treatment. But this large foundation of evidence allows us to look patients in the eye and say testosterone therapy does not appear to increase risk of prostate cancer over a moderate duration.” Of significant importance in this study was most men received injections, as opposed to topical creams which do not always reach therapeutic blood levels, and had follow-up tests that proved that their testosterone levels actually rose with the therapy.
https://www.ncbi.nlm.nih.gov/pubmed/29933385
Here’s a lengthy detailed review by the Mayo Clinic on the possible risks of TRT – for men and women – but for those who just want the take home: “We agree with the current opinions of the AACE/ACE, the FDA, as well as the international expert consensus panel that testosterone treatment should be considered for symptomatic men with clinically confirmed hypogonadism, that there is no compelling evidence that testosterone therapy either increases or decreases CVD risk, and that testosterone therapy for men with testosterone deficiency is effective, rational, and evidence based. The benefits of treatment of low testosterone levels with testosterone therapy in men and women substantially outweigh any risks, according to the current data.” I highly recommend giving this a read as it also elucidates many of the flaws of the anti-trt cohort studies.
https://www.mayoclinicproceedings.org/article/S0025-6196(17)30824-8/fulltext
Does standard TRT cause an increased risk of heart attack? This retrospective cohort study compared the rate of myocardial infarction (heart attack) against 414,000 men treated with testosterone. No significant correlation was found between men treated with testosterone and heart attack. Within physiological ranges, testosterone treatment has no cause for concern when it comes to life-long CV health. In fact, TRT has been shown to improve multiple health parameters over the long-term. “This large, retrospective, real-world observational study showed no significant association between testosterone therapy (TT) use and acute myocardial infarction (MI) when comparing TT-treated with untreated hypogonadal men overall, by age, or by prior cardiovascular disease (CVD).”
http://www.societaitalianadiendocrinologia.it/public/pdf/bellastellanovembre2017.pdf
One of the most inflammatory studies against TRT was the 2017 JAMA study by Matt Budoff. In this article, Dr. Jeffrey Dach takes a “critical look” at the assessments made in the Budoff study that testosterone increases atherosclerotic plaque formation. It is my assessment that Budoff had come to some conclusions that were not warranted given his research.
Injections are not only safer, they are more effective than topical patches or creams. “Intramuscular TRT is more effective than transdermal formulations at increasing LBM and improving muscle strength in middle-aged and older men, particularly in the lower extremities.”
https://www.ncbi.nlm.nih.gov/pubmed/29542875
At physiological levels, testosterone is safe and exerts a beneficial effect on myocardial function including mechanisms at cellular and mitochondrial level.
https://www.ncbi.nlm.nih.gov/pubmed/29978359
Weight loss and treatment to replace testosterone levels improve the metabolic profile and quality of life in patients with obesity and hypogonadism; these beneficial effects depend on treatment modality and duration of therapy. The use of testosterone replacement therapy may be indicated, as it has not been shown to increase cardiovascular risk, and retrospective studies suggest a reduction in events in men with metabolic syndrome and type 2 diabetes.
https://www.ncbi.nlm.nih.gov/pubmed/29974886
Testosterone replacement therapy has the potential to alleviate some of the morbidity associated with hypogonadism and metabolic syndrome.
https://www.ncbi.nlm.nih.gov/pubmed/28202344
In otherwise healthy obese men with mild to moderate symptoms and modest reductions in testosterone levels, testosterone treatment improved androgen deficiency symptoms over and above the improvement associated with weight loss alone, and more severely symptomatic men achieved a greater benefit.
https://www.nature.com/articles/ijo2016242
“There is no credible evidence to indicate that T therapy increases the risk of CVD. On the contrary, testosterone therapy may be protective. The scientific evidence shows that restoration of physiological levels of T are critical for maintaining men’s health. Interestingly, T therapy has been used as early as 1940s with no reported adverse effects on the CV system. On the contrary, T therapy has been shown to improve the symptoms of angina pectoris and peripheral vascular disease. A spectrum of recent studies (Table below) have shown that T therapy does not increase the risk of CVD.”
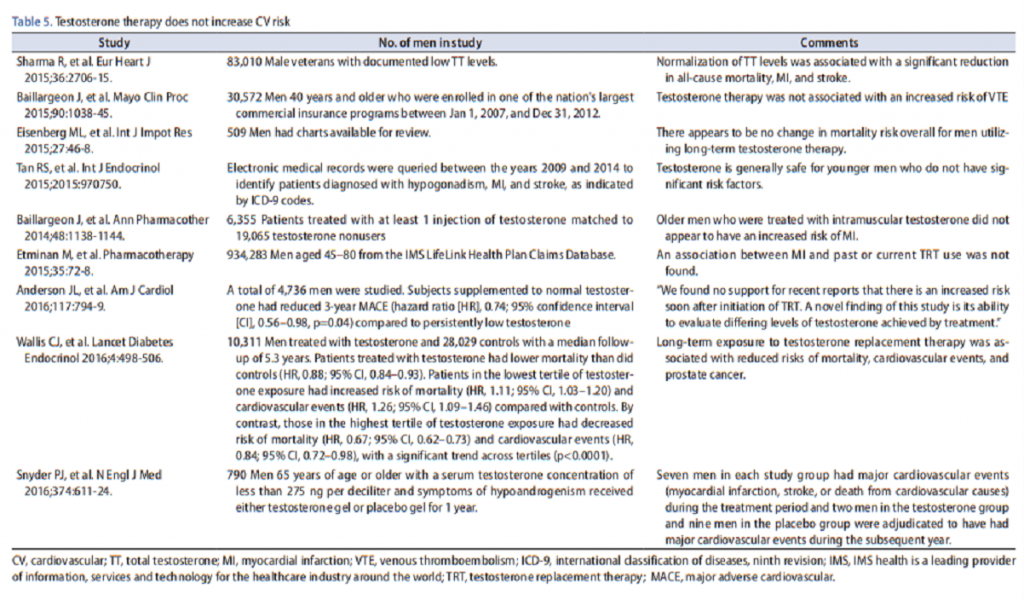
“A wealth of recent studies demonstrated that T therapy in men with testosterone deficiency (TD) is associated with increased lean body mass, reduced fat mass and waist circumference, improvement in glycemic control, and reduced obesity. T therapy is also associated with improvements in lipid profiles, amelioration of metabolic syndrome (Met S) components, reduced inflammatory biomarkers, reduced systolic and diastolic blood pressure, and improvements in sexual function. More importantly, T therapy is associated with amelioration of diabetes and reduced mortality. However, few studies, marred with serious methodological and analytical flaws, suggested that T therapy is associated with increased cardiovascular (CV) risk. As summarized in this review, a thorough and critical analysis of these studies showed that the risks purported are unsubstantiated and such studies lacked credible scientific and clinical evidence. Moreover, recent observational, registry studies, clinical trials, and meta-analyses, all revealed no increase in CV risks in men receiving T therapy. In this review, the benefits of T therapy in adult men with TD and the lack of credible evidence suggesting that T therapy is linked to increased CV risks are discussed. It should be noted that the literature is replete with studies demonstrating beneficial effects of T therapy on CV and overall health.”
https://www.ncbi.nlm.nih.gov/pubmed/27488887
Long-term TRT in men with hypogonadism and a history of CVD appears to be an effective approach to achieve sustained improvements in anthropometric parameters and cardio-metabolic function, with no reported increases in CVD events. The fact that none of these high-risk patients had another CV event may suggest that TRT can have beneficial effects in men with a history of CVD, provided comprehensive secondary prevention therapy is already in place. In men with testosterone deficiency and a history of cardiovascular disease, who received testosterone therapy for up to 8 years, no patient suffered a major adverse cardiovascular event during the full observation time.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4913536/
This study was conducted to examine the association between testosterone therapy and new myocardial infarction (MI) and stroke events in a series of patients treated at Low T Centers across the United States, consisting of mainly young (mean age = 46), otherwise, healthy men. 19,968 met eligibility criteria for receiving testosterone treatment. There was no evidence of worsening preexisting MI or stroke in patients treated with testosterone.
http://dx.doi.org/10.1155/2015/970750
A retrospective cohort study was conducted within an integrated health care delivery system. Men at least 40 years old with evidence of androgen deficiency either by a coded diagnosis and/or a morning serum total testosterone level of less than 300 ng/dL were included. The eligibility window was January 1, 1999, to December 31, 2010, with follow-up through December 31, 2012. Among men with androgen deficiency, dispensed testosterone prescriptions were associated with a lower risk of cardiovascular outcomes over a median follow-up of 3.4 years. The cohorts consisted of 8808 men (19.8%) ever dispensed testosterone (ever-TRT) (mean age, 58.4 years; 1.4% with prior cardiovascular events) and 35 527 men (80.2%) never dispensed testosterone (never-TRT) (mean age, 59.8 years; 2.0% with prior cardiovascular events). Median follow was 3.2 years in the never-TRT group vs 4.2 years in the ever-TRT group.
https://www.ncbi.nlm.nih.gov/pubmed/28241244
“Analysis included 31 randomized controlled trials published between 2010 and 2018. Retrieved trials included 2675 and 2308 patients in TRT and placebo groups, respectively. The analysis documented that TRT was not associated with an increased cardiovascular (CV) mortality or morbidity either when overall or major adverse CV events were considered.”
https://www.tandfonline.com/doi/abs/10.1080/14779072.2018.1510314
Low Testosterone level has implications for metabolic health in both males and females and should be considered a risk factor because of its correlation with metabolic syndrome and all-cause mortality. Androgen therapy in men with T deficiency improves physical efficiency and reduces the risk of re-hospitalization.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6299269/
“Supplementation of Testosterone and resistance training in older men with low–normal levels does not appear to improve or harm vascular function.”
https://www.physiology.org/doi/abs/10.1152/japplphysiol.00165.2018